1. Introduction
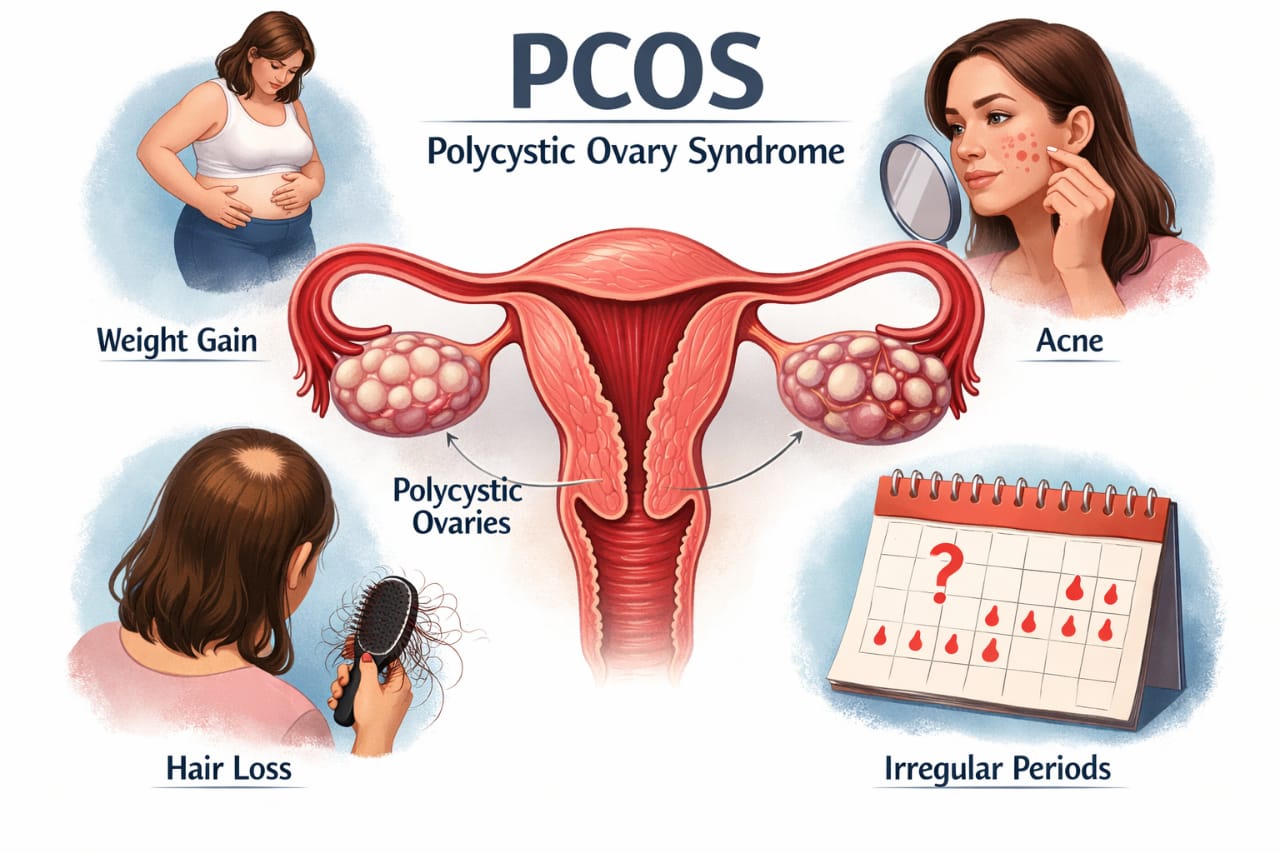
PCOS has also emerged as one of the major endocrine problems being witnessed in the reproductive-aged population of females. It is estimated that PCOS affects millions of woman worldwide and is recognized for being associated with lifestyle diseases.
“PCOS belly,” which refers to an accumulation of fat in the lower abdominal region due to a build-up of visceral fat, can be a difficult symptom for women with PCOS to deal with.
PCOS belly is a concern not only because of the looks it can give the individual but also by the hormonal changes it can cause on a regular basis. This can be detrimental to the potential future health of the person. This topic describes PCOS belly and the effects it can cause. It also provides tips on home management of the condition based on WHO recommendations.
2. What Is a PCOS Belly?
PCOS belly is referred to as the accumulation of fat around the lower abdomen, which is usually observed in women who have Polycystic Ovary Syndrome. Such fat accumulation is also referred to as central or abdominal obesity, which is more harmful than fat accumulation in other parts of the body.
Common Characteristics
- Protruding or distended abdomen
- Trouble losing intra-abdominal fat while on a diet
- Weight gain, primarily mid-section obesity
- Higher waist-to-hip ratio
That fat is visceral fat and is mainly deposited around vital organs, thereby accelerating possible cases of diabetes.
3. What Causes Belly Fat in PCOS?
PCOS belly occurs due to a combination of hormonal imbalance, metabolic disorders, and lifestyle factors. This has been identified under WHO’s Non-Communicable Disease risk factors.
3.1 Insulin Resistance
Many women with PCOS have insulin resistance. The World Health Organization accepts insulin resistance as an important cause of obesity, type 2 diabetes, and metabolic syndrome.
In PCOS:
- The body does not respond to insulin correctly
- Insulin levels in the blood increase
- Too much insulin stimulates fat accumulation, particularly in the abdominal region
- Insulin promotes androgen synthesis by the ovaries, bringing about more PCOS symptoms
3.2 Hormonal Imbalance
Furthermore, women with PCOS tend to have high levels of androgens, or male hormones like testosterone, impacting their fat distribution.
As a result:
- Fat accumulates in the abdominal area rather than in hips or legs
Other hormonal imbalance side effects include:
- Irregular menstrual cycles
- Acne and excess body hair
- Trouble with weight control
3.3 Chronic Low-Grade Inflammation
WHO states that chronic inflammation of the body is also known to be a cause of metabolic disorders. In PCOS, chronic low-grade inflammation may cause:
- Enhanced insulin resistance
- Encouraged fat accumulation
- Increased difficulty with weight loss
Visceral inflammation is directly associated with health risks for PCOS.
3.4 Sedentary Lifestyle
According to WHO, physical inactivity is among the top risk factors for deaths worldwide.
- Slows metabolism
- Decreases insulin sensitivity
- Increases abdominal fat deposition
Increasing central obesity can be observed in physically inactive women with PCOS.
3.5 Stress and Cortisol
Stress leads to an increased production of cortisol in the body, and cortisol is very closely linked with fat accumulation around the waist.
Stress related to PCOS symptoms, infertility, or body image issues may exacerbate PCOS-related belly problems.
4. Primary Symptoms of Other Conditions in PCOS
4.1 Irregular Menstrual Cycle
- Irregular periods
- Less than 8 periods per year
- Long cycles
- Amenorrhea
Triggered by irregular ovulation.
4.2 Symptoms of Excess Androgens
- Excess facial hair (upper lip, chin, jaws)
- Hair growth on chest, stomach, back
- Oily skin
- Dermatological issues
- Thinning scalp hair or hair loss
4.3 Polycystic Ovaries
- Larger ovaries
- Several small follicles (cysts)
Remark: According to WHO, cysts are not required for the diagnosis of PCOS.
4.4 Weight Gain and Weight Loss Challenges
- Abdominal weight gain
- Resistance to weight loss
- Greater waist circumference
4.5 Insulin Resistance and Blood Sugar Issues
- Increased appetite and sugar cravings
- Fatigue after meals
- Dark skin patches (acanthosis nigricans)
- Type 2 diabetes or prediabetes
4.6 Skin Changes
- Persistent acne
- Darkened, thickened skin
- Skin tags
4.7 Fertility Issues
- Delayed ovulation
- Irregular or anovulatory ovulation
- Difficulty with conception
4.8 Pelvic Pain (Some Women)
- Mild pelvic pain
- Lower abdominal discomfort
4.9 Mental Health and Mood Changes
- Anxiety
- Depression
- Low self-esteem
- Mood swings
- Body image issues
4.10 Sleep Problems
- Poor sleep quality
- Insomnia
- Increased risk of sleep apnea
4.11 Fatigue and Low Energy
- Constant fatigue
- Trouble focusing
- Daytime sleepiness
5. Health Risks Associated with PCOS Belly
WHO reports:
“Abdominal obesity is a more serious problem than obesity in general.”
5.1 Major Health Risks
- Type 2 diabetes
- Cardiovascular diseases
- Metabolic carrier states
- Mental health disorders
6. WHO Guidelines for Dealing with PCOS Belly
6.1 Nutritious and Balanced Diet
Foods to Include:
- Whole grains
- Fruits and vegetables
- Lean proteins
- Healthy fats
Foods to Limit:
- Sugary drinks
- Ultra-processed foods
- Excess salt and trans-fatty acids
6.2 Physical Activity (WHO Guidelines)
- 150–300 minutes of moderate activity weekly
- Muscle-strengthening activities at least 2 days per week
6.3 Maintain Healthy Body Weight
Weight loss of as little as 5–10% improves:
- Insulin resistance
- Menstrual regularity
- Visceral fat levels
6.4 Reduce Sedentary Behavior
- Standing breaks
- Walking after meals
- Staying active in daily activities
6.5 Stress Management and Mental Well-being
- Mindfulness
- Yoga
- Adequate rest
6.6 Sleep Needs
- 7–9 hours per night
- Normal sleep patterns
7. Medical Support When Required
Doctors may recommend:
- Thiazolidinediones
- Hormonal therapies
- Monitoring blood glucose and cholesterol levels
8. Common Myths Regarding PCOS Belly
Myth: PCOS belly is due to overeating alone
Fact: Hormonal and metabolic problems play a prominent role
Myth: Crash dieting is the answer
Fact: WHO advises against extreme dietary measures
Myth: Exercise alone can treat PCOS
Fact: A holistic lifestyle approach is needed to adopt sustainable practices
9. Lifestyle Changes to Live Healthily with PCOS
WHO adopts a life-course perspective on women’s health:
- Focus on health rather than perfection
- Be patient with progress
- Seek professional help when needed
10. Conclusion
PCOS belly is a physical display of hormonal imbalance, closely linked to insulin resistance, obesity, and other factors delineated by the WHO. Though it may have dangerous health implications, PCOS belly can be thoroughly managed through healthy eating, exercise, stress management, appropriate sleep, and medical attention when required.
To address PCOS belly and PCOS overall, lifestyle changes rather than quick fixes have proven effective. Educating women with accurate information remains the strongest tool for improving PCOS outcomes.
[…] Cortisol raises blood sugar by increasing glucose production in the liver. High cortisol levels are directly linked to insulin resistance, especially in winter.This mechanism is also seen in hormonal conditions such as PCOS. […]