1. Introduction
Orthostatic hypotension is a common but often overlooked blood pressure condition that can significantly affect daily life. It usually occurs when a person stands up from a sitting or lying position and suddenly feels dizzy, lightheaded, or weak. Many people ignore these symptoms, assuming they are normal, but untreated orthostatic hypotension can increase the risk of falls, injuries, and reduced quality of life. In this blog post, we will discuss orthostatic hypotension in detail, including its ICD-10 code, causes, risk factors, symptoms, and effective lifestyle changes to manage it.
2. What is Orthostatic Hypotension?
Orthostatic hypotension, also known as postural hypotension, is a condition in which blood pressure drops suddenly when a person changes position, especially when standing up. Normally, the body adjusts blood pressure quickly to maintain adequate blood flow to the brain. In Postural Hypotension, this adjustment does not happen properly, leading to reduced blood flow to the brain and causing symptoms like dizziness or fainting.
3. ICD-10 Classification of Postural Hypotension
The ICD-10 code for orthostatic hypotension is I95.1. This code is used by healthcare professionals for medical records, diagnosis, billing, and insurance purposes. Proper use of the ICD-10 code for Postural blood pressure drop helps in accurate documentation and better treatment planning.
4. Common Causes of Postural Hypotension
There are several causes of orthostatic hypotension, and they can vary from person to person. Common causes include dehydration, prolonged bed rest, blood loss, and disorders of the nervous system. Conditions such as diabetes, Parkinson’s disease, and heart problems can also interfere with blood pressure regulation. In some cases, orthostatic hypotension may be caused by medications or age-related changes in the body.
5. Risk Factors for Postural Hypotension
Certain factors increase the risk of developing orthostatic hypotension. These include older age, chronic illnesses, dehydration, and prolonged immobility. People with diabetes, heart disease, or neurological disorders are at higher risk. Pregnancy and extreme heat exposure can also contribute to the development of orthostatic hypotension.
6. Common Signs and Symptoms
The most common signs and symptoms of Orthostatic blood pressure drop include dizziness, lightheadedness, blurred vision, weakness, nausea, and headache. Some people may feel unsteady or confused after standing up. These symptoms usually last for a few seconds to minutes and often improve after sitting or lying down.
7. Severe and Warning Symptoms to Watch For
In severe cases, Postural Hypotension can cause fainting (syncope), chest pain, shortness of breath, or difficulty concentrating. These warning symptoms should not be ignored, as they may indicate a serious underlying condition. Frequent falls or loss of consciousness require immediate medical attention.
8. Difference Between Orthostatic blood pressure drop and Hypotension
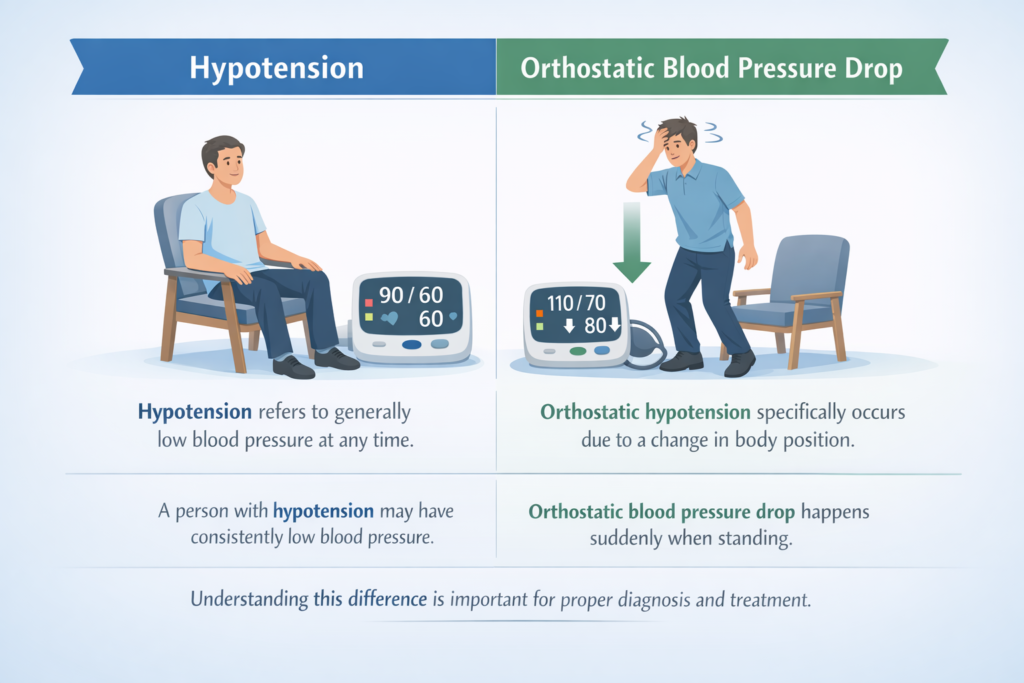
Hypotension refers to generally low blood pressure at any time, while orthostatic hypotension specifically occurs due to a change in body position. A person with hypotension may have consistently low blood pressure, whereas Orthostatic blood pressure drop happens suddenly when standing. Understanding this difference is important for proper diagnosis and treatment.
9. Postural Hypotension in Elderly Patients
Postural Hypotension is more common in elderly patients due to age-related changes in blood vessels and reduced baroreceptor sensitivity. Older adults are also more likely to take multiple medications and have chronic illnesses, which increases their risk. In elderly patients, Postural Hypotension can lead to falls, fractures, and loss of independence.
10. Postural Hypotension Related to Medications
Many medications can contribute to orthostatic hypotension. These include blood pressure medicines, diuretics, antidepressants, antipsychotics, and medications used for Parkinson’s disease. Alcohol can also worsen symptoms. Medication-related orthostatic hypotension should be reviewed by a healthcare provider to adjust doses or switch drugs if necessary.
11. Lifestyle Changes to Manage Orthostatic Hypotension
Lifestyle changes play an important role in managing orthostatic hypotension. Drinking enough fluids, increasing salt intake (if advised by a doctor), standing up slowly, and wearing compression stockings can help. Regular physical
12. When to See a Doctor
You should see a doctor immediately if:
You experience frequent dizziness or lightheadedness when standing
Symptoms of Orthostatic Hypotension are getting worse over time
You have fainting (syncope) episodes or near-fainting spells
Dizziness is accompanied by chest pain, shortness of breath, or blurred vision
You feel confused or weak after standing up
Falls occur due to sudden drops in blood pressure
Older adults, people with diabetes, heart disease, Parkinson’s disease, or those taking blood pressure medications should be especially cautious. In such cases, Orthostatic Hypotension may signal an underlying medical condition that needs proper evaluation.
It is also important to consult a doctor if symptoms appear after starting a new medication, as some drugs can trigger or worsen Orthostatic Hypotension.
Early diagnosis helps prevent complications like injuries from falls, reduced quality of life, and long-term cardiovascular issues. With the right treatment plan, Orthostatic Hypotension can be managed effectively.
13. FAQs
1. Is Postural hypotension a serious condition?
Orthostatic Hypotension can be mild or serious depending on the cause. Occasional symptoms may not be dangerous, but persistent or severe cases can increase the risk of falls, fainting, and injuries. That’s why medical advice is important if symptoms are recurring.
2. Can Orthostatic Hypotension go away on its own?
Yes, in some cases Postural hypotension may improve with proper hydration, lifestyle changes, and medication adjustment. However, if it is caused by a chronic condition, long-term management may be required.
3.When should Orthostatic Hypotension be treated as an emergency?
If Postural hypotension causes repeated fainting, chest pain, severe weakness, or injury from falls, seek emergency medical care immediately.
